What is it about?
Many UK general medical practitioners (GPs) have accepted the evidence that probiotcs can reduce the incidence and severity of antibiotic diarrhoea. However, there is growing evidence for their benefits in other clinical circumstances: irritable bowel syndrome, inflammatory bowel disease, eczema, protection against some cancers and control of diverticular disease. Therefore we invited all GPs in the English county of Surrey to complete an online questionnaire in which we suggested a variety of clinical scenarios in which they might advise the patient to take a course of a daily probiotic. GPs varied in their experience and opinion as to whether advice to take a probiotic would be appropriate in these scenarios, with the choice of the option ‘frequently advise’ varying from 63% (recurrent vaginal candidiasis) to 1% (to reduce the risk of bowel and bladder cancer). 13% of participants said they would frequently advise a course of probiotics foir patients with diverticulitis and pyrexia and 32% said they would occasionally do so.
Featured Image
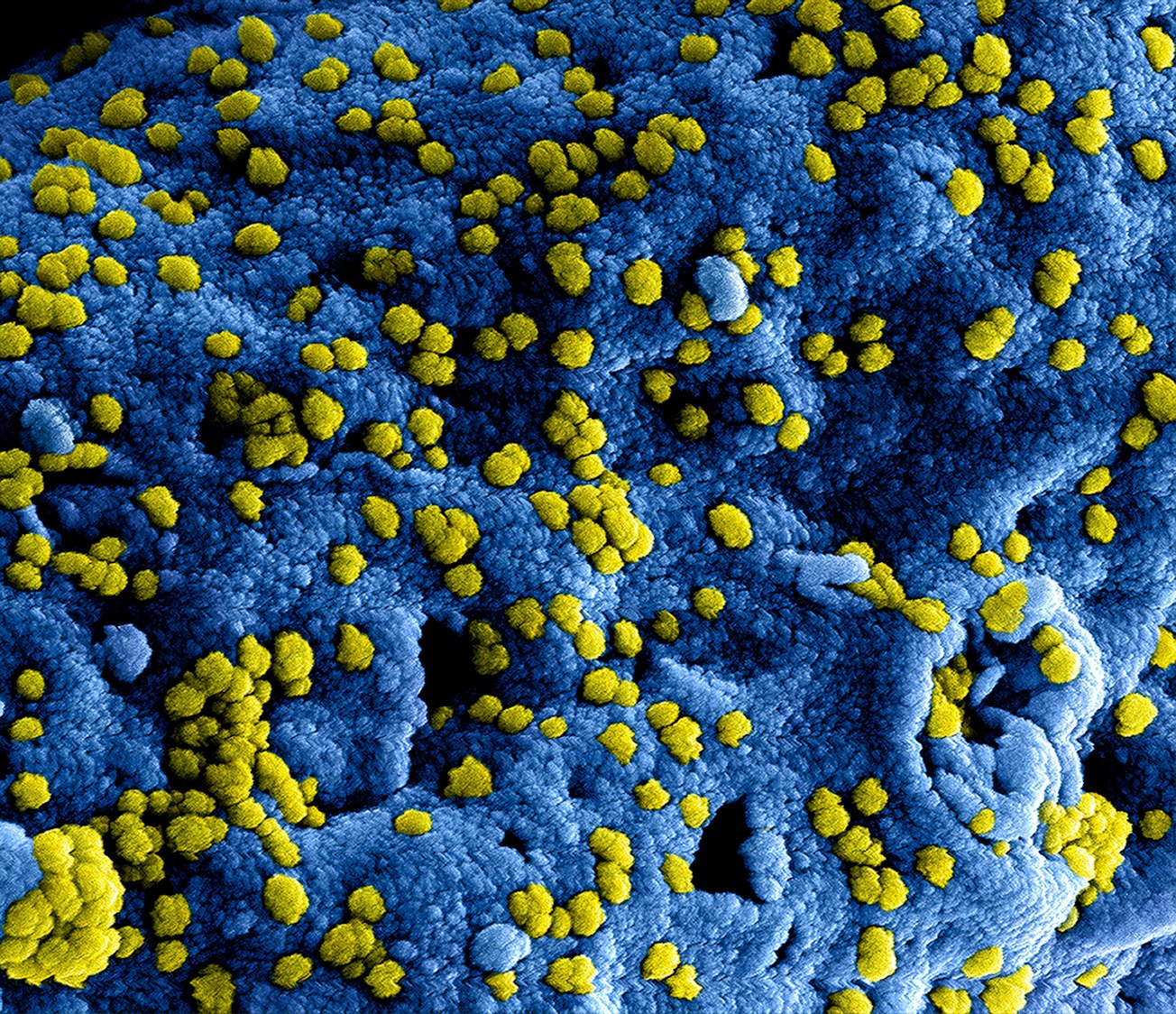
Photo by CDC on Unsplash
Why is it important?
Advising on probiotics by GPs seems to have reached a tipping point. Guidelines for on advice to their patients about probiotic consumption would be helpful. This should include advice on the timing of the probiotic dose when given concurrently with antibiotics and the ideal number of days for a probiotic course in different clinical circumstances.
Perspectives
I followed up this paper with further research on the use of probiotics in management of diverticular disease but when it came to publication of my results, I got stung. The first seven journals I submitted to turned me down and on referee commented that I should not be using the term "probiotic" as it had been rejected by the European Union!
Dr John Anthony Alvan Nichols
Royal Society of Medicine
Read the Original
This page is a summary of: A web questionnaire to determine the advice general practitioners give on probiotics, Journal of Nutritional & Environmental Medicine, January 2005, Taylor & Francis,
DOI: 10.1080/13590840600692980.
You can read the full text:
Contributors
The following have contributed to this page







