What is it about?
In this study we asked ourselves whether it’s possible to improve one of the earliest discovered natural antibiotics, bacitracin. Short answer, yes! Below, the path to our “next-generation bacitracins.” History: In 1943 bacteriologist Balbina Johnson identified a new antibiotic substance produced by a strain of bacillus bacteria that had been isolated from an infected wound in the leg of a young patient. That patient’s name: Margaret Tracy. Fast forward a few short years to 1948 and the FDA approved this new antibiotic for therapeutic use. The antibiotic was named bacitracin, a combination of “Bacillus” and “Tracy,” in honour of the patient’s name. Clinical use: Due to uncertainties related to bacitracin’s safety and efficacy, it found its primary use as a topical antibiotic. For decades, bacitracin has been marketed in combination with other anti-infectives in the over-the-counter ointments Neosporin and Polysporin. Mechanism of action: In 1973 Daniel Storm and Jack Strominger experimentally demonstrated that bacitracin targets and kills bacterial cells by specifically binding to the phospholipid undecaprenyl pyrophosphate, commonly called C55PP. Forty years after the work of Storm and Strominger, the team of Nicoleta Economou, Simon Cocklin, and Patrick Loll published the first crystal structure of the complex formed between bacitracin and C55PP. The crystal structure reported by the Loll group revealed that upon binding to C55PP, certain parts of the bacitracin molecule align to form a “hydrophobic face” proposed to interact with the bacterial membrane.
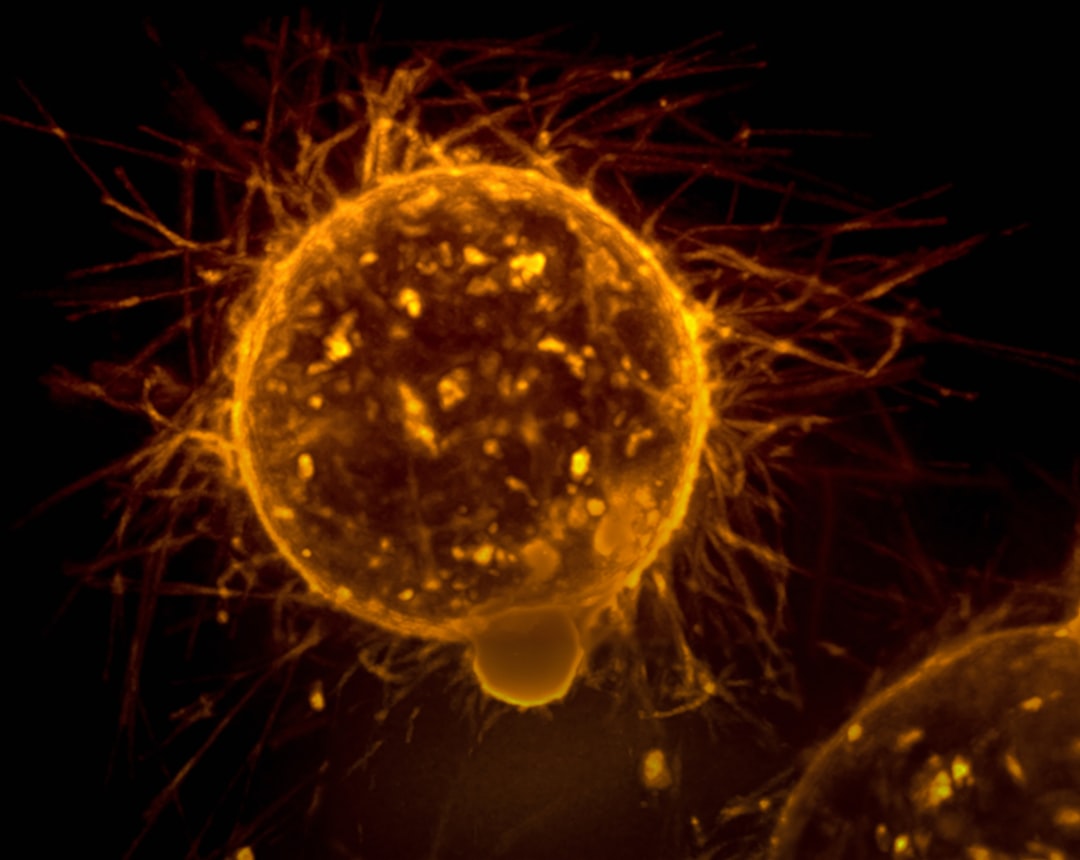
Featured Image

Photo by Adrian Lange on Unsplash
Why is it important?
Our idea: Inspired by Loll group's structure, we designed a series of new bacitracin analogues to investigate whether it's possible to further enhance the hydrophobic interactions between bacitracin and the bacterial surface as a means of increasing antibacterial activity. Using solid phase peptide synthesis we prepared “next-generation bacitracins” and tested their activity against a panel of clinically relevant pathogens. We found that a number of these new bacitracin variants do indeed possess dramatically enhanced antibacterial activities!
Perspectives
Of particular note was the finding that our most active next-generation bacitracin analogues are highly effective at preventing the growth of dangerous vancomycin-resistant enterococci (VRE) strains. Our understanding of this particularly potent anti-VRE activity is a question for future research but for now we are intrigued by the potential for such compounds to be used in treating VRE infections. Special credit to lead author Ned Buijs for driving the project forward along with great collaborations with the groups of Tanja Schneider (University of Bonn) and Stephen Cochrane (Queen's University Belfast). We're also thankful for the support our research group benefits from as a member of the Leiden Early Drug Discovery and Development hub (LED3) and the Institute of Biology Leiden (IBL).
Nathaniel Martin
Universiteit Leiden
Read the Original
This page is a summary of: A classic antibiotic reimagined: Rationally designed bacitracin variants exhibit potent activity against vancomycin-resistant pathogens, Proceedings of the National Academy of Sciences, July 2024, Proceedings of the National Academy of Sciences,
DOI: 10.1073/pnas.2315310121.
You can read the full text:
Contributors
The following have contributed to this page